The Journey Continues (Journey Part 2)
Now that we've covered the road to my POTS diagnosis and connection to online support groups, the journey continues... After my positive tilt table test, I had no idea what came next for me. Just the regimen of medication and increasing my salt and water intake.
First things first, trying to drink a gallon of water a day is no easy task. My doctor recommended Gatorade because my body would do a better job of hanging onto it than it would with plain water. Plain water, means I'm peeing within about 5 minutes of drinking it. I quickly learned that Gatorade powder is a lot cheaper than buying it premixed.
My nausea had not subsided at all and I was still experiencing presyncopal (nearly passing out) episodes upon standing.
Flornef did not work for me and Metoprolol was making me even more nauseous. My friend told me to contact my doctor about the side effects because every POTS patient reacts differently to the medications or that it would be smart to get an anti-nausea medication. I had NO idea that I could get a prescription for anti-nausea medication. I immediately called my GP's (General Practioner) office, only to find she wasn't there. They put me on hold and I waited for the on-call doctor. They sent in a prescription to my pharmacy and I tried it out for a week. Only to find I was extremely lethargic and something didn't feel right.
I looked up side effects/drug interactions online - turns out the anti-nausea medication (I can't for the life of me remember what it was called) had an amplifying effect with metoprolol and was lowering my blood pressure. Keep in mind my normal blood pressure was only 90/60. I immediately discontinued the anti-nausea medication.
At this point my symptoms weren't improving and I was frustrated. Again, I turned to my friend. She recommended seeing a Neurologist because the root cause of POTS is a neurological condition.
I went back to my GP and asked for a referral. Then I counted the days until my appointment (roughly 3 weeks).
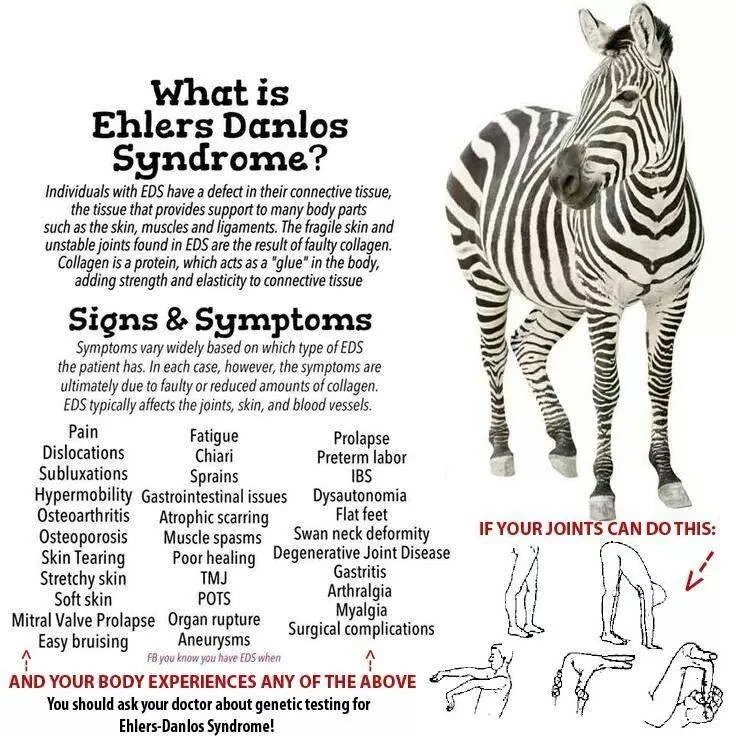
Only to be extremely disappointed. The doctor was great but didn't specialize in Dysautonomia (umbrella term for when your body doesn't properly regulate things that are supposed to be automatic - POTS falls under this umbrella). Luckily she knew exactly where I needed to go and made a referral over to that clinic.
I waited another 2.5 months for this appointment.
While I waited, I finally splurged and bought myself an Omron at home Blood Pressure cuff. I needed to know what was going on and why I wasn't feeling better. My blood pressure had stayed just as low as it had before (and occasionally dipped lower - because of the metoprolol), despite my increased fluid intake. I got really sick.
Bedridden again. It was the heat of another humid Wisconsin summer and I wasn't coping well. I ended up not taking my medications because they just made me feel worse. After I was done being sick, I called my cardiologist and said I felt better off the medications than I did while I was taking them. We discontinued the Metoprolol because my body clearly wasn't tolerating it well. He then turned all of my care over to the doctors at the Dysautonomia clinic because he said they would have a better understanding of the care that I needed.
It was worth the wait and the drive! Luckily it was only about a 45 minute drive. I finally found doctors that understood me. An entire staff that was warm, welcoming, and understood the struggle to find my diagnosis. My doctor (Dr. Rose Dotson) ran some in office tests and I came back positive for Small Fiber Neuropathy (a defect in my small sensory nerve fibers that handle pain and temperature sensing). I talked to her about my Flornef prescription and how I had thrown up a few times after taking it and that I wasn't feeling any better when it did go down. We discontinued Flornef and decided to try Midodrine. I told her about my nausea and how it hadn't improved.She prescribed Zofran 8mg dissolving tablets that I could take as needed so I could finally get some relief. She used to work at the Mayo Clinic and ordered a series of very specific blood tests (developed at Mayo). We scheduled a follow up appointment in about a month, to check the progress of the Midodrine. She also ordered a gastric emptying test (odd test, I'll explain later) because of my nauseousness after eating. Some of the blood work I had done that day. The rest of the blood work had to wait because I needed to get to work.
I was now just on the Midodrine, Zofran, and tracking my blood pressure and symptoms. Still no change. My blood pressure still didn't increase.
I went to the clinic not far from house to have the blood draws done. Big mistake. I should have gone back to the other clinic, even if it was an additional 35 minutes away. There were very specific instructions for how it needed to be collected. They were testing for catecholamines which change depending on if you're laying down or standing. I sat in the waiting area of this busy clinic for about 35 minutes, then they took me back to an exam room. I explained that I needed to lay down for 10 minutes before they could draw my blood. They left me back there for 30 minutes and never checked on me. I couldn't get up because then this whole process would have to start over. I called the clinic from my cell phone and told them the situation. It was awkward. They were not good at their jobs. The phlebotomist looked at the orders and started grabbing all the tubes she would need, I stopped counting at 14. I pass out at the sight of my own blood, I was not looking forward to this. She read the specific instructions from Dr. Dotson and proceeded to draw all of the viles...while I was laying down. Turns out the results of all this blood work were invalid. Half of them were supposed to be taken while I was laying down and the other half while I was standing. I wasted about 2 hours of my time. (I still, 2 years later, need to go back and have this testing redone...). So roughly 15 viles of blood, a hot summer day, and a car without air conditioning TERRIBLE idea on my part because humid heat is a trigger for me to pass out. I was so loopy and nauseous. I took a Zofran and at least the nausea subsided enough that I didn't puke. After all of this, I went to work...luckily I wasn't late.
Next was my gastric emptying test. I wasn't allowed to eat beforehand but the test was early in the morning. I got there, they brought me back and it was time to eat radioactive (seriously, not a joke.) scrambled eggs and wash it down with juice. Then they proceeded to take a standing X ray and told me to go to the waiting room and they would come get me for the next scan. This process repeated several times...standing scan, freezing waiting room...standing scan, freezing waiting room...I don't remember how long the intervals between scans were but I was there for at least a few hours. The worst part of this test was the waiting, it was so cold I remember shivering. It was the middle of summer, I had not dressed for an arctic waiting room.
I was still monitoring my blood pressure, no improvement there.
My follow up appointment was with Mary Yellick NP (she is Dr. Dotson's nurse practioner). We talked about my at home blood pressure readings and how I was feeling. Mary increased the frequency of my Midodrine dose to 3 times daily to see if spacing it out would help since there was no improvement. The results of my Gastric Emptying study came back that I had 'borderline delayed gastric emptying'...whatever that meant. It meant further testing - she ordered an Upper Endoscopy. My bloodwork still hadn't come back from the Mayo Clinic (and now I realize that those results are worthless anyway because my blood wasn't taken properly. Eventually they did arrive though and came back normal).
The thought of an Upper Endoscopy scared the crap out of me. They put you under sedation while they stick a camera down your throat, take pictures, and a biopsy. I had never been put under anesthesia before and I knew that my dad had woken up during his pacemaker replacement surgery. YIKES! My girlfriend at the time and I hadn't been dating very long (hadn't even become official yet) and I had to rely on her for a ride to and from the procedure. If she didn't come through, I'd have to cancel the procedure.
The morning of the procedure I wasn't allowed to eat, again. *Seems to be a theme with most of my testing* My girlfriend came and picked me up and we went to the clinic for the procedure. She reassured me that I'd be okay but I was still freaking out on the inside. We checked in and they asked what her "relationship" was to me, my girlfriend froze and I replied with partner (we joked about this for the next year of our relationship). They took us back and I changed into the lovely hospital gown (I swear they don't fit anyone and they're so uncomfortable. They were going down my throat, why did I need a hospital gown? Why couldn't I just wear my own clothes?). They brought me back and I got on the hospital bed. They put an IV in my hand and hurriedly were talking about things between themselves. Then the anesthesiologist randomly appeared at the head of my bed and asked how I was feeling. I said I felt normal and he took this as a need to push more of the sleepy time drugs into my hand. I didn't feel any different after the second round, he checked the IV in my hand, adjusted it (yanked and re-stuck in my vein)...and I don't remember anything until I woke up. They put me in a recovery area near the nurses station and I proceeded to talk the nurse's ear off about my master's degree/future career aspiration of reducing childhood obesity in the inner city (this would change after I finally received all of my diagnoses to helping other people with my conditions to not have to wait this long to get a diagnosis). After my philosophical discussion with the nurse about how childhood obesity in the inner city is a systemic problem and not an individual one...I was wheeled out to the waiting area. Where my 'partner' was waiting for me. We giggled about it for a while. The waiting area was strange it felt like a home for the elderly. The chairs were the weird reclining hospital chairs (the kind you'd see sitting next to a hospital bed). I drank some coffee and the nurse said we could leave whenever I felt ready. We stayed for about 30 minutes and I was ready to get out of there.
The results of my upper endoscopy didn't really show much of anything. Everything was healthy and we didn't need to worry at least from the stomach up.
So I'll end this post here with a quick recap:
- Meds - Midodrine 3x daily, Zofran as needed (usually daily)
- Blood pressure still not where it should be
- Gastric Emptying - borderline delayed
- Upper Endoscopy - normal
- Blood tests - pointless because they took them incorrectly
**Connect with me on Facebook or Twitter** Or send me an email below